
Yellowstone Conference: Stronger Together, Building Strategic Partnerships for Lasting Impact
Join us for a day of inspiration, learning, and collaboration designed to strengthen partnerships and spark lasting impact.
Yellowstone Conference 2025 at a Glance:
Topic: Stronger Together, Building Strategic Partnerships for Lasting Impact
Date: Thursday, October 2, 2025
Time: 8:30 AM – 4:30 PM
Location: 1701 Ray of Hope Lane, Billings, MT.
Tickets: Click here to purchase tickets on Eventbrite
Credits: 5.75 CEUs & 6 OPI credits available
Format: In-Person or Virtual | Lunch & Snacks Provided
This annual gathering unites leaders, innovators, and changemakers from across sectors to exchange ideas, celebrate successes, and spark new opportunities for growth. Through dynamic panel discussions and interactive networking, participants will gain practical tools, fresh perspectives, and stronger connections to drive meaningful, lasting impact in our communities.
Panel Topics & Descriptions
Strengthening Native American Partnerships: Leveraging Community Partnerships for Collective Impact
Moderator: Josie Brady, Native American Services Coordinator.
Panelists: Clint Valandra, Indigenous Education Coordinator, Billings Public Schools | Charlene “Charli” Sleeper, Founder, MMIP Billings Advocacy Project; Mental Health Worker, Yellowstone Boys and Girls Ranch | Sunny Day Real Bird, Director of American Indian Outreach, Montana State University Billings | David R. Blaine, CEO, Crow Times Youth and Elder Works
This panel emphasizes the importance of building strong, respectful, and mutually beneficial relationships with Native American communities. By fostering authentic partnerships, the effort seeks to honor cultural traditions, elevate community voices, and collaborate on shared goals. Leveraging cross-sector partnerships enhances access to resources, supports sustainable solutions, and drives collective impact. The focus is on long-term trust, equity, and shared decision-making to strengthen outcomes for Native youth in their communities.
Empowering Excellence: Strengthening Workforce Development through Higher Education Partnerships
Moderator: Kristin Thompson, Associate Director of Human Resources.
Panelists: James C. Petrovich, PhD, MSW, Professor & Department Chair; Founding Director, Master of Social Work Program, Carroll College | Kate Chapin, MSW, LCSW, Executive Director, Center for Children, Families, and Workforce Development, University of Montana | Becky Lyons, EdD, Director of Career & Employment Services, Montana State University Billings | Jen Chancellor, MBA, University Development Counselor, Grand Canyon University
A strong, mission-aligned workforce is the backbone of effective nonprofit impact. This panel explores how strategic partnerships with higher education institutions can help build and sustain a pipeline of skilled, passionate professionals. These partnerships not only enhance organizational capacity but also ensure that services remain responsive, community-centered, and future-focused. Together, we can cultivate a workforce that’s ready to meet today’s needs—and tomorrow’s possibilities.
Mission-Driven Collaboration: Uniting Youth-Serving Organizations for Greater Reach
Moderator: Katie Gerten, Marketing & Communications Director.
Panelists: Matt Leavenworth, PhD, LCPC, Founder, Pay Love Forward; Vice Chair, Yellowstone County Suicide Prevention Coalition | Nina Hernandez, Executive Director, Friends of the Children – Eastern Montana; Nonprofit Leader & Consultant | Dennis Sulser, EdD, Retired CEO, Youth Dynamics; 40-Year Education & Healthcare Leader | Sarah Music, Director of Coordinated School Health, Montana Office of Public Instruction
When youth-serving organizations unite around a shared mission, their impact multiplies. By combining strengths and resources, partners expand reach and deepen support for kids and families. These collaborations close gaps and build stronger systems—especially in under-resourced areas—creating a more connected, resilient network of care that ensures youth get the support they need, when they need it.
Bridging Sectors, Building Futures: Public-Private Partnerships for Sustainable Change
Moderator: Mike Chavers, CEO.
Panelists: Sierra Riesberg, Social Services & Behavioral Health Systems Leader | Erika Purington, MS, CEO, Allies in Aging; Leadership Coach & Nonprofit Executive | Matt Bugni, CEO, AWARE | Meghan Peel, Interim Division Administrator, Behavioral Health & Developmental Disabilities Division, Montana DPHHS | Kirsten Smith, MPA, PMP, Principal, Bloom Consulting, LLC
When government, business, and community organizations come together, the results can be transformative. This panel explores how cross-sector collaboration sparks innovation, drives sustainable solutions, and strengthens communities for the long term.
Special Keynote Speaker
Mohini Venkatesh, Chief of Staff of the National Council for Mental Wellbeing
Conference Agenda
- Registration (8:30–9:00 AM)
- Welcome (9:00–9:15 AM)
- Strengthening Native American Partnerships Panel (9:15–10:30 AM)
- Break (10:30–10:45 AM)
- Empowering Excellence Panel (10:45–12:00 PM)
- Lunch (12:00–1:00 PM)
- Mission-Driven Collaboration Panel (1:00–2:15 PM)
- Dessert Break, Sponsored by Grand Canyon University (2:15–2:30 PM)
- Bridging Sectors, Building Futures Panel (2:30–3:45 PM)
- Keynote Speaker – Mohini Venkatesh (3:45–4:30 PM)
Have Questions About the Yellowstone Conference?
For questions about this event, please reach out to us at info@ybgr.org.
Stay Connected
Stay tuned to our news updates for the latest from across Montana, and follow us on social media. You can find us on LinkedIn at Yellowstone Boys and Girls Ranch, Instagram at @ybgr_cares, and Facebook at Yellowstone Boys and Girls Ranch.

Lasting Legacy of Giving: The Story Behind Donald Nutter Memorial Dining Hall
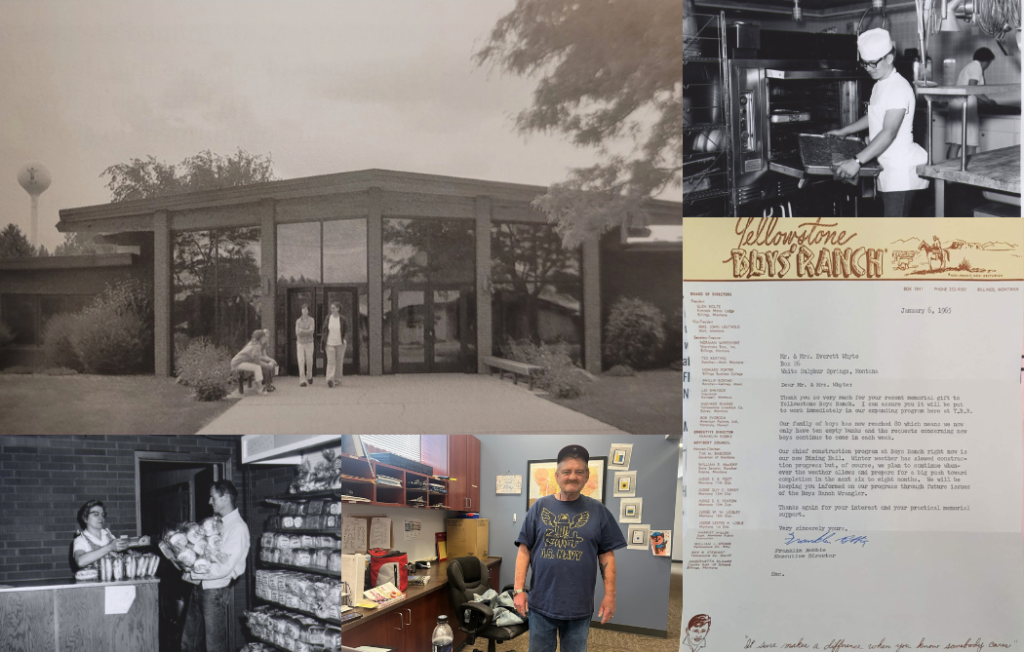
Can a $1 gift make a difference? At Yellowstone Boys and Girls Ranch, it always has.
From a heartfelt donation in 1964 to the hundreds of meals served each day with care, the story of Donald Nutter Memorial Dining Hall is one rooted in generosity, community, and small acts that build something lasting.
This beloved space at the Ranch stands today thanks to the many who gave—each gift, large or small, helped bring it to life.
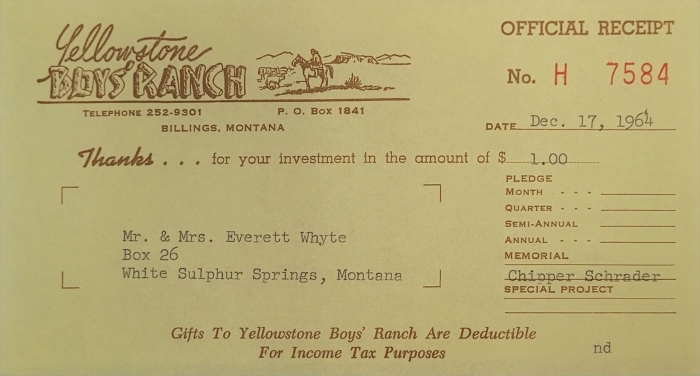
A powerful reminder of that came recently from John Whyte, our Admissions Coordinator in Great Falls. John shared a thank-you letter his parents received in 1965 from then-CEO Franklin Robbie, recognizing their $1 donation toward the Dining Hall’s construction.
Honoring a Tradition of Gratitude
A single dollar and a sincere note of gratitude. It’s a tradition the Yellowstone Foundation proudly carries on today—still sending handwritten thank-you letters to the donors who help power our mission.
Every gift matters. Every act of generosity leaves a mark.
A Space Built for Community, Nourishment, and Care
Named after Governor Donald Nutter, a Montana leader instrumental in the Ranch’s early years, the Dining Hall officially opened in 1966. That day, 450 people gathered to celebrate a new chapter—one centered around shared meals, belonging, and care.
Before the Ranch had a chapel, the Dining Hall served as a sacred space where kids gathered for Sunday morning services. It also became a cozy movie theater for monthly film nights, filling the room with laughter and community.
Still Feeding Hearts and Lives Today
Today, the Donald Nutter Memorial Dining Hall remains a cornerstone of daily life at the Ranch. The Sodexo team prepares and serves hundreds of meals each day, ensuring every child in our care is well-nourished and supported.
More than just a building, the Dining Hall is a symbol of what’s possible when people come together to give, build, and believe. It’s a space shaped by love, filled with stories, and sustained by the ongoing generosity of those who stand behind our mission.
Learn More About Our History
Visit our History page to explore the story—and the caring people—who gave birth to our mission. Their vision continues to touch the lives of thousands of youth across Montana and beyond each year.
Want to dive deeper? You can also find A Legacy of Caring, written by our founder, Franklin Robbie, on Amazon.

14 Quotes on Parenting When Triggered

What does it mean to parent when triggered? Often, our kids meet us with big emotions and behaviors that can stretch us and activate an in-kind response, particularly when we’re stressed or worn thin.
And at that moment, we’re challenged to slow down. To create space between our reaction and response so we can respond in love.
Below are fourteen quotes to help you with parenting when triggered.
Quotes on Parenting When Triggered
Quote 1: Kids don’t “make” us yell. They reveal to us where we have room to grow, where we have wounds to heal, and where we still have unresolved trauma from our own childhoods. – Inspired by Shelly Robinson
Quote 2: When the milk is splattered all over the floor, and those little eyes are looking at you for your reaction, remember what really matters. It takes 5 minutes to clean up spilled milk; it takes much longer to clean up a broken spirit. – Rebecca Eanes
Quote 3: Unless there is a risk of your child hurting themselves and you need to step in, when your child is having a meltdown or “tantrum,” your first step should be to calm yourself down. Very rarely does effective parenting happen when you are triggered, angry, or stressed. – @australianpsychologist
Quote 4: Your capacity to have empathy for your child in difficult moments is directly related to your capacity to have empathy for yourself in difficult moments. – @drnicolebeurken
Quote 5: In the heat of the moment, first, attend to how your child’s behavior makes you feel, so you can then attend to how your child feels without the interference of your own emotions. – @dr.siggie
Quote 6: When I calm myself first, I protect my kids from things that have nothing to do with their behavior. – Inspired by Dr. David Erickson
Quote 7: When your child is having a meltdown, your number one priority is to stay in control of your own emotions. – @dr.siggie
Quote 8: Your child’s state of reactivity will often mirror your own state of reactivity. – Inspired by Caley Kukla
Quote 9: Meeting a child’s hostility with adult aggression only adds fuel to the fire. To extinguish hostile behavior, meet it with calm and compassion. – Rebecca Eanes
Quote 10: It doesn’t make sense that adults lose control with children for losing control. And then expect children to be able to control themselves when the adult in front of them can’t even control themselves. – Inspired by Jessica Martin-Weber
Quote 11: My kids aren’t to blame for triggering me, pushing my buttons, or driving me up the wall. It’s on me to work through those triggers, remove those buttons, and tear down the wall instead of expecting my kids to change their behavior before I change mine. – Inspired by Iris Chen
Quote 12: If we want our kids to stop and think before reacting, then we need to show them how. That means we need to practice pausing, keeping ourselves regulated, and then responding—not just with them, but in all areas of life. – @drnicolebeurken
Quote 13: Peaceful parenting isn’t about your ability to stop feeling what you feel. It’s about separating your feelings from your actions. Letting the feelings come. Acknowledging them. Letting them go. Then responding with intention. – @loveandletgrow
Quote 14: Respond to children with the same connection and empathy for all their behaviors, and they’ll know your love isn’t conditional. That’s how you become their “safe space.” – Sarah R. Moore
Want More?
Check out the rest of our blog and follow us on social media. You can find us on LinkedIn at Yellowstone Boys and Girls Ranch, Instagram at @ybgr_cares, and Facebook at Yellowstone Boys and Girls Ranch.
Yellowstone Academy: A School Built on Belief and Possibility
Built from scratch. Backed by belief.
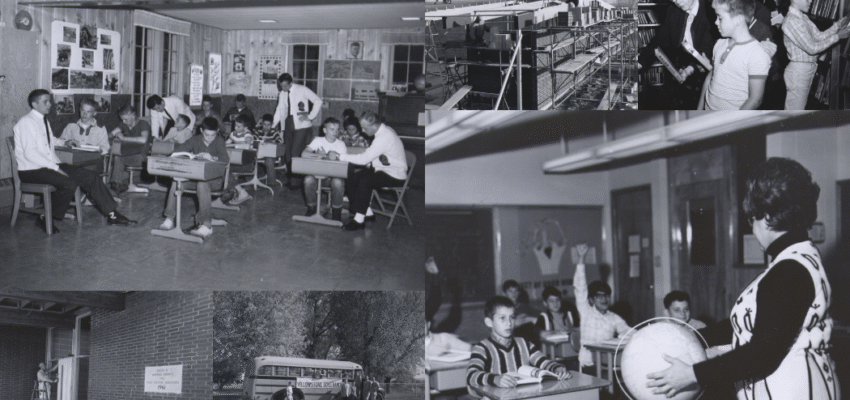
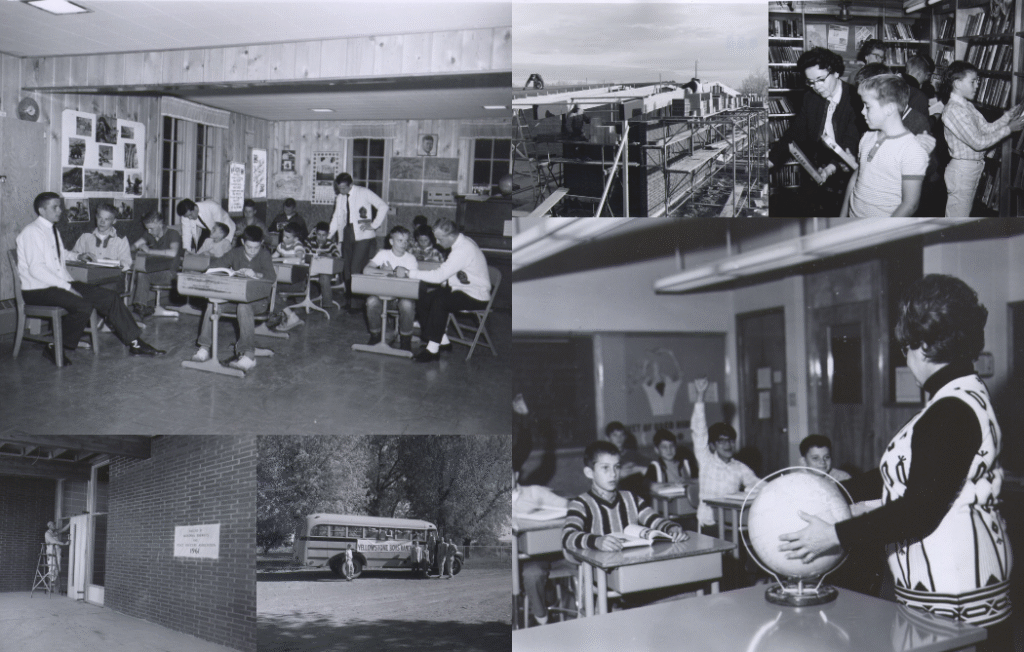
Yellowstone Academy began with salvaged desks, a makeshift classroom, and a simple but powerful vision: a place where every child has the chance to learn, heal, and grow. That first classroom marked a defining chapter in Yellowstone Academy history.
In 1959, inside a lodge furnished with desks from an abandoned schoolhouse, the vision came to life. The small space filled quickly with students who had experienced trauma, struggled in traditional classroom settings, and needed a different kind of learning environment—one grounded in patience, structure, and hope.
Students soon outgrew the space, overwhelming the nearby rural school system. It was clear that a new model of education was needed.
A “School Without Failure”
In 1961, generous local businesses stepped in with time, talent, and donated materials to help create what became known as a “school without failure”—a place where success was possible for children who had long felt left behind.
As one parent shared at the time:
“I’ve seen such a great change in my son. It’s the first time he’s been successful in a classroom—and received an A.”
Laying the Foundation for the Future
By September 16, 1965, School District 58 was officially established, allowing education and healing to grow hand in hand. What began as a four-room schoolhouse expanded through the generosity of caring donors such as Alvy Casper and the Heptner sisters, whose gifts helped create additional classrooms, an auditorium, and space for community day treatment.
In 1962, fifteen students proudly graduated from eighth grade—many for the first time in their lives. It was more than a graduation. It was proof that belief, structure, and opportunity could change a child’s path.
Yellowstone Academy History — A Legacy That Continues Today
Today, Yellowstone Academy continues to carry their original vision forward, writing the next chapter of Yellowstone Academy history each day. With small class sizes, individualized instruction, therapeutic support, and caring adults who meet students where they are, the Academy remains a place where youth rediscover their potential.
What began with salvaged desks and unwavering belief continues to transform lives—one student at a time.
Learn More About Our History
Visit our History page to explore the story—and the caring people—who gave birth to our mission. Their vision continues to touch the lives of thousands of youth across Montana and beyond each year.
Want to dive deeper? You can also find A Legacy of Caring, written by our founder, Franklin Robbie, on Amazon.
Trauma-Informed Communication Starts With L.O.V.E
Trauma-informed communication isn’t just about what we say—it’s about how we say it. It’s about presence, intention, and connection, especially in moments that feel charged or difficult.
That’s where L.O.V.E. comes in.
It’s a simple framework that reminds us to slow down and center ourselves when communicating—whether with kids, colleagues, or loved ones. And in high-stress moments, that pause can make all the difference.
The L.O.V.E. Approach to Trauma-Informed Communication
When emotions run high, try using the L.O.V.E. approach:
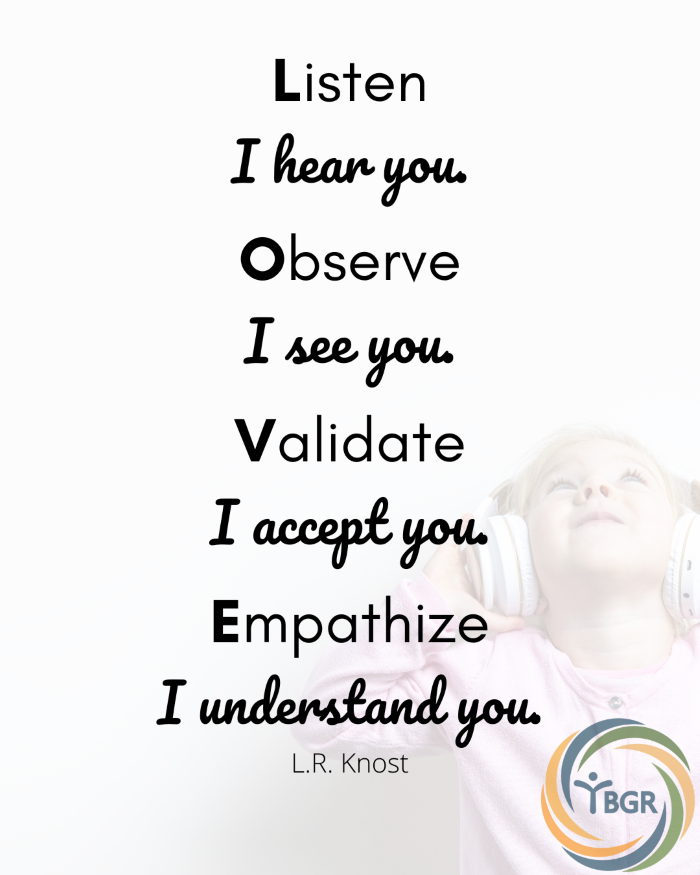
L – Listen (“I hear you.”)
Give your full attention. Put away distractions, pause your inner dialogue, and truly listen—without interrupting or planning your response. Feeling heard is the foundation of connection.
O – Observe (“I see you.”)
Notice more than words. Body language, tone, and facial expressions often speak louder. Observation helps us tune in to what might be happening beneath the surface.
V – Validate (“I accept you.”)
Validation isn’t agreement—it’s acknowledgment. It means recognizing someone’s feelings as real and important, even if you don’t fully understand or share them.
E – Empathize (“I understand you.”)
Empathy invites us to step into another’s shoes and connect with their experience. It’s how we show care, build trust, and respond rather than react.
Learn More: 15 Quotes on Communicating with Empathy
Slow Down to Strengthen Connection
We can avoid so many problems when we respond with L.O.V.E. instead of reacting in haste.
In trauma-informed communication, timing matters. When emotions are high, it’s okay—even wise—to pause. Whether you’re parenting, leading a team, or resolving conflict with a friend, take a moment to check in with yourself before diving into tough conversations.
Give yourself permission to delay. The goal isn’t just to get through it—it’s to move forward in a way that builds connection, not tension.
Want More?
Check out the rest of our blog and follow us on social media. You can find us on LinkedIn at Yellowstone Boys and Girls Ranch, Instagram at @ybgr_cares, and Facebook at Yellowstone Boys and Girls Ranch.

Yellowstone County organizations requesting community help this back-to-school season
How Yellowstone Academy’s Vo-Tech Program Took Root
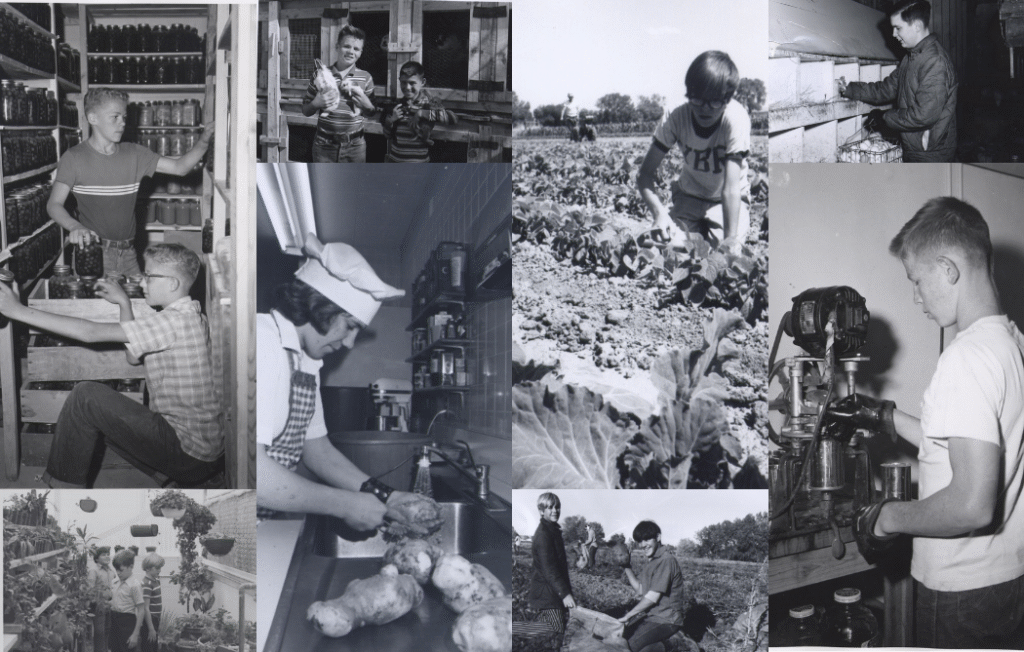
Knowledge that sticks. Work that matters.
In Yellowstone Academy’s Vo-Tech program (Vocational Technologies), students don’t just learn skills—they build purpose. Many kids who come to the Ranch arrive discouraged, behind in school, or unsure of their own abilities. Vo-Tech gives them a way to reconnect with learning in a way that feels real.
A Program Rooted in Hands-On Learning
The Vo-Tech program began taking shape in 1972, when Yellowstone Academy launched its first vocational curriculum. Just two years later, the Academy earned state accreditation, marking a turning point. For the first time, students were gaining hands-on experience connected to life, work, and a future they could build for themselves.
That vision grew again in 2005, when Bob McFarlane—long-standing member of the YBGR family and Yellowstone’s first superintendent—led students and volunteers in rebuilding a donated greenhouse. Their efforts created the 13,000-square-foot Poetzl Horticultural Center, a space designed for learning through doing.
Today, the Poetzl Horticultural Center is central to the Vo-Tech experience. The greenhouse operates as a pheasant hatchery, with birds later moving to flight pens built by students. Kids raise bees for honey, grow fruit for jams and pies, and tend to chickens, corn, pumpkins, beans, and squash.
The land is a living classroom—one where confidence grows alongside the crops.
Building Skills That Last
Yellowstone Academy’s Vo-Tech program is more than a set of classes. It’s an opportunity for students to build something that lasts—on the land, in the shop, and within themselves.
Students also learn trades such as small engine repair, welding, and woodworking. These hands-on skills introduce new strengths, build vocational confidence, and help students experience the pride that comes from meaningful work.
What they build stays with them.
Learn More About Our History
Visit our History page to explore the story—and the caring people—who gave birth to this mission. Their vision continues to touch the lives of thousands of youth across Montana and beyond each year.
Want to dive deeper? You can also find A Legacy of Caring, written by founder Franklin Robbie, available on Amazon.

4 Tips for Building Meaningful Relationships

A recent study by Cigna found that more than 50% of Americans experience loneliness, and 54% say they don’t have anyone in their lives who truly knows them.
In today’s fast-paced world, building meaningful relationships isn’t always easy—but it’s essential for both mental and physical health.
If you’re looking for practical ways to feel more connected, here are four simple strategies to help you create stronger, healthier bonds with others.
#1: Spend Time with the People Who Matter
In the busyness of everyday life, it’s easy to overlook the people who mean the most. But even fifteen minutes of intentional time with someone you care about can have a powerful impact.
Prioritize presence.
#2: Eliminate Distractions
To truly connect, be all in. Put down your phone, turn off notifications, and focus on who you’re with. We build meaningful relationships when we listen fully and show others they matter.
#3: Embrace Solitude to Strengthen Self-Connection
To connect deeply with others, we must first know ourselves. Spend time alone in ways that feel fulfilling, whether it’s walking in nature, journaling, or listening to music.
A healthy relationship with yourself sets the tone for every other connection.
#4: Be Kind—and Take the First Step
Kindness creates space for trust. Share encouragement, check in on someone, or offer help when it’s needed. Strong relationships grow when we let others know they’re seen and valued.
Building meaningful relationships takes effort, but it’s worth it. Small steps can lead to deeper, more fulfilling connections with others and with yourself.
Want More?
Check out the rest of our blog and follow us on social media. You can find us on LinkedIn at Yellowstone Boys and Girls Ranch, Instagram at @ybgr_cares, and Facebook at Yellowstone Boys and Girls Ranch.

YBGR Group Homes Collaborate, Bringing Billings and Great Falls Teams Together

When YBGR group homes collaborate, the impact goes beyond logistics—it strengthens teams, improves communication, and enhances the care we provide to Montana kids.
That collaboration was on full display this month as staff from River’s Edge and STAR Group Homes in Billings traveled to connect with the team at North Skyline Group Home in Great Falls.
A Day of Purposeful Collaboration—and Tacos
Hosted by the North Skyline crew, the gathering included therapeutic discussion, relationship-building, and a taco lunch that brought everyone together. From shared care strategies to laughter over homemade fry bread, the event reinforced the value of taking time to connect as a united team.
Moments like these show how YBGR group homes collaborate not only to solve challenges, but to support one another and align around our shared mission: caring people, preparing youth for life.
Strengthening Teams & Care Across Montana
Teammates in attendance included: Jessie Wilson, Michelle Mouat, Lori Kapphan, Chloe Foster, Dani Miller, Brittany Olson, Zander Mathis, Richard Heusel, Jennifer Hawks, Alycia Hall, and Mariah Lefebre.
As YBGR continues to grow across the state, collaboration between group homes plays a critical role in maintaining consistency, trust, and mission-focused care. When we invest in each other, everyone benefits—especially the youth we serve.
At YBGR, the strength of our teams is the foundation for the care we provide.
Stay Connected
Stay tuned to our news updates for the latest from across Montana, and follow us on social media. You can find us on LinkedIn at Yellowstone Boys and Girls Ranch, Instagram at @ybgr_cares, and Facebook at Yellowstone Boys and Girls Ranch.

15 Quotes on Communicating with Empathy

Empathy is more than kindness—it’s the ability to understand and share in what someone else is feeling. Whether you’re leading a team, raising a child, or simply navigating day-to-day interactions, communicating with empathy builds trust, eases tension, and strengthens relationships.
Below are 15 quotes to inspire deeper connection through communication with care.
How to Connect with Empathy
Quote 1: It’s extremely powerful to hear someone say, “I get you. I understand. I see why you feel this way.” This kind of empathy disarms us. – Inspired by Daniel J. Siegel

Quote 2: People will hear you better if you speak from a voice of compassion instead of authority. They long to be understood more than to be lectured. – Inspired by Dodinsky
Quote 3: Sometimes, the most influential thing we can do is listen. – Bob Burg
Quote 4: What does it mean to “hold space” for someone else? It means that we are willing to walk alongside another person in whatever journey they’re on without judging them, making them feel inadequate, trying to fix them, or trying to impact the outcome. When we hold space for other people, we open our hearts, offer unconditional support, and let go of judgment and control. – Unknown
Quote 5: Connection: The power that exists between people when they feel seen, heard, and valued. – Brene Brown
Quote 6: When someone is struggling, they already know. They don’t need advice. They don’t need solutions. They don’t need judgment. What they need are a smile and grace. And to be reminded that the person behind the battle can still be loved. – Lauren Fortenberry
Quote 7: Empathy has no script. There is no right way or wrong way to do it. It’s simply listening, holding space, withholding judgment, emotionally connecting, and communicating that incredibly healing message “you’re not alone.” – Brene Brown
Quote 8: I judge others less when I judge myself less. – Unknown
Quote 9: When someone shares a difficult situation they are facing, don’t respond as though life is simple and there’s an easy solution. Life is complex, and often there are no simple solutions. – Rachel Samson
Quote 10: What people of all ages can use in a moment of distress is not agreement or disagreement; they need someone to recognize what it is they’re experiencing. – Adele Faber
Quote 11: Trauma happens and harms us. But I often wonder if the worst trauma is the second wave—when your story is disbelieved, mistrusted, and maligned. May your story find safe harbor in the presence of people who will honor both your vulnerability and resilience. – @kjramseywrites
Quote 12: To empathize with someone’s experience, you must be willing to believe them as they see it and not how you imagine their experience to be. – Brene Brown
Quote 13: Client: I know I probably shouldn’t have these feelings. Therapist: What you are feeling in this situation is perfectly okay. – Rachel Samson
Quote 14: Do not try to reason with someone who is not regulated. – Inspired by Rachel Samson
Quote 15: One of the most effective strategies for regulating emotion is cultivating an attitude of acceptance towards your emotions and the emotions of others. – Rachel Samson
Want More?
Check out the rest of our blog and follow us on social media. You can find us on LinkedIn at Yellowstone Boys and Girls Ranch, Instagram at @ybgr_cares, and Facebook at Yellowstone Boys and Girls Ranch.
